Keratoconus
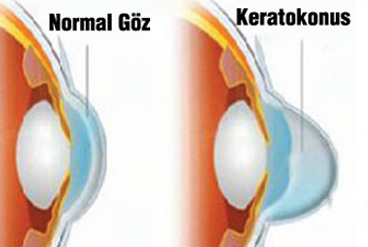
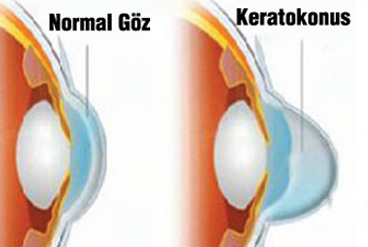
Keratoconus is a progressive eye disease in which the normally round cornea thins and begins to bulge into a cone-like shape. This cone shape deflects light as it enters the eye on its way to the light-sensitive retina, causing distorted vision. Keratoconus can occur in one or both eyes and appears in the teens or early twenties.
As a progressive eye disease, it may progress for 10-20 years and then slow or stabilize. Further progression of the disease may require surgery including transplantation of the cornea. But if keratoconus is successfully managed with a variety of clinical and surgical techniques, there will be little or no impairment to the patient's quality of life. A person who has progressive nearsightedness and irregular astigmatism should visit an ophthalmologist if she/he also experiences additional problems with blurred vision. Lack of knowledge often creates fear. Patients should learn all about this condition. They should ask questions and discuss their concern with doctors and others who have keratoconus. From an emotional and psychological standpoint, it is important to understand the nature of keratoconus.
The weakening of the corneal tissue that leads to keratoconus may be due to an imbalance of enzymes within the cornea. This imbalance makes the cornea more susceptible to oxidative damage from compounds called free radicals, causing it to weaken and bulge forward.
Genetic predisposition, overexposure to ultraviolet rays from the sun, excessive eye rubbing and a history of poorly fit contact lenses can be also risk factors.
13% of patients have other family members with the disease.
Keratoconus can be difficult to detect, because it usually develops so slowly. However, in some cases, it may proceed rapidly. As the cornea becomes more irregular in shape, it causes progressive nearsightedness and irregular astigmatism to develop, creating additional problems with distorted and blurred vision. Glare and light sensitivity also may be noticed. Keratoconic patients often have prescription changes every time they visit their eye care practitioner. It's not unusual to have a delayed diagnosis of keratoconus, if the practitioner is not familiar with the early-stage symptoms of the disease.
The eye examination may proceed to measurement of the localised curvature of the cornea with a manual keratometer with detection of irregular astigmatism suggesting a possibility of keratoconus.
A more definitive diagnosis can be obtained using corneal topography, in which an automated instrument projects the illuminated pattern onto the cornea and determines its topology from analysis of the digital image. The topographical map indicates any distortions or scarring in the cornea.
In the early stages, vision can be corrected with glasses or regular soft contact but as disease progresses they are not able to correct the distortion caused by the irregular corneal surface and more complex contact lens designs are required.
Rigid Gas Permeable contact lense s are primary option for correcting keratoconus vision. The rigid lens masks the underlying irregular cornea and functions as the new refractive surface of the eye, with the tear film filling in the space between the back of the contact lens and the front of the eye.
There is no one “best” lens for keratoconus. The “best lens” is the one that fits your eye, corrects your vision and is comfortable to wear.
Recently tiny plastic inserts are placed just under the eye's surface in the periphery of the cornea and help re-shape the cornea for clearer vision. Several studies also showed that Intacs can improve visual and also have the advantage of being removable and exchangeable. The surgical procedure takes only about 10 minutes. Intacs might delay but can't prevent a corneal transplant if keratoconus continues to progress.
Some people with keratoconus can't tolerate a rigid contact lens, or they reach the point where contact lenses or other therapies no longer provide acceptable vision. The last remedy to be considered may be a cornea transplant. Over 90 per cent of corneal transplants done for keratoconus continue to allow good vision at five years post-transplant. But even after a transplant, you most likely will need glasses or contact lenses for clear vision
Last Updated: October 23, 2024



























